For children

For adults

Tongue-Ties


WHAT is pediatric Sleep Disordered breathing?
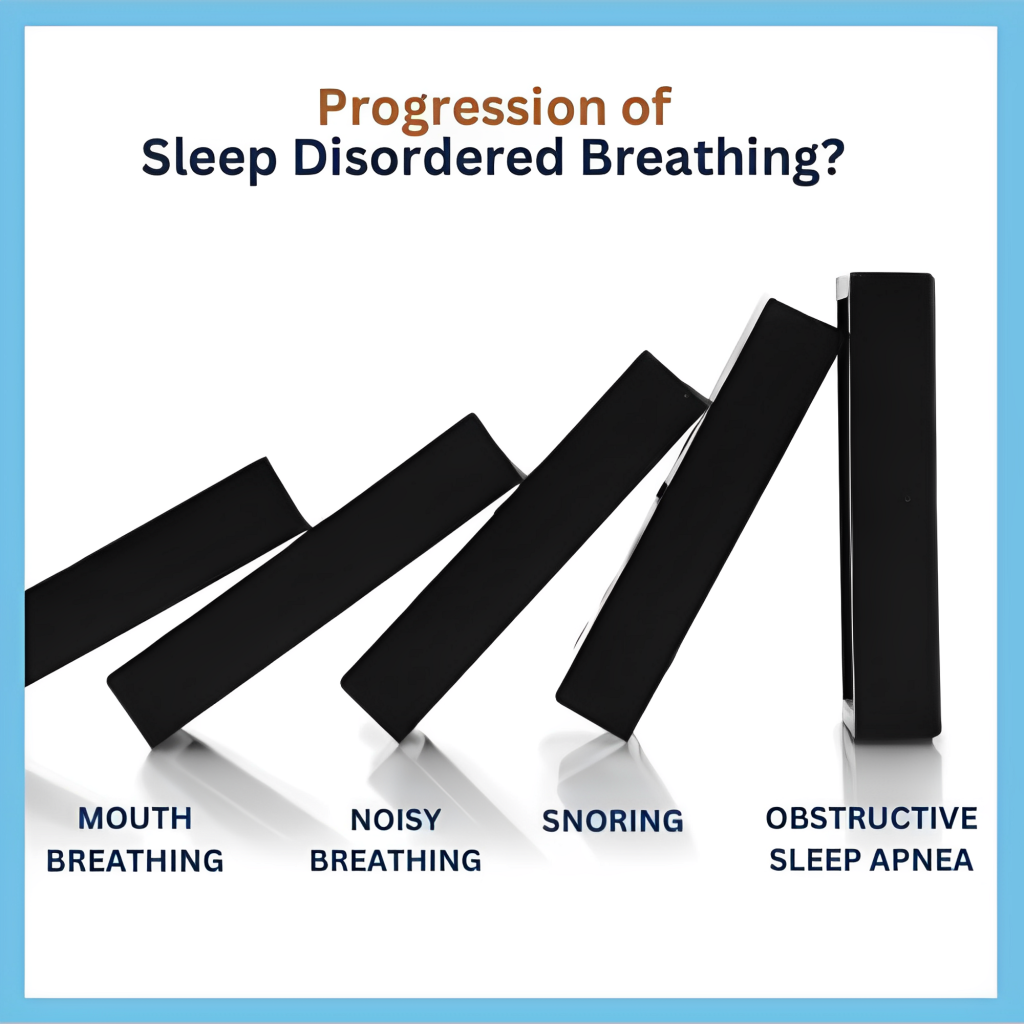
Normal breathing during sleep should be through the nose, silent and with lips closed. If your child is mouthbreathing, have noisy breathing, snoring or grinding their teeth, they may suffer from Sleep Disordered Breathing.
Unfortunately this disease is a spectrum and tends to get worse over time.
Why does Sleep Disordered Breathing matter ?
A variety of problems that were once unassociated with sleep disorders, can often be linked back to airway issues and poor sleep, such as…
These issues can escalate when you don’t treat the root cause. In fact, untreated sleep and breathing disorders can negatively impact a child’s IQ every year it’s left unattended.

How do we evaluate ?
In her practice, Dr. Rokadia does a detailed evaluation of your childs craniofacial growth and development. Looking at nasal breathing, tongue function, presence of tongue-ties, swallow patterns, size of the jaws and palate, grinding of teeth, size of tonsils etc helps her create a treatment plan that addresses root causes.
With her extensive training and personal commitment to alleviating this problem, Dr. Rokadia has developed protocols that determine the causes and effects of sleep-disordered breathing and developmental growth problems, helping many children finally get the sleep they need.
How do we treat SDB in children?
Dr. Rokadia treats children who are 4 years old and above. However, she also sees 3-year-olds for evaluations to help chart a path for future treatment and to prevent issues from arising.
Treatment varies in each case but usually involves myofunctional therapy in correlation with a myofunctional appliance and breathing re-education. Depending on the situation, interceptive orthodontics and release of any tethered oral tissues (lip ties and tongue ties) may also be needed.
Treatment is usually 1-2 years in time.
Aim of our treatment is to establish nasal breathing , reduce future airway and breathing issues, and reduce the need for extensive orthodontics in later years.
We listen with our hearts and can help you make the changes you need to transform the health of your child.
WHAT IS OBSTRUCTIVE SLEEP APNEA?
Obstructive sleep apnea or OSA is a sleep disorder that is caused by a collapsing of the soft tissues at the back of the throat. Patients with sleep apnea can experience a range of symptoms, but most report feeling tired, groggy and fatigued much of the time. Sleep apnea can affect anyone, even children. Diagnosis and effective treatment can be both life-changing and life-saving.
Common signs of sleep apnea can include:
WHAT IS UPPER AIRWAY RESISTANCE SYNDROME?
UARS is a less recognized form of sleep disordered breathing. Patients tend to be younger and non-obese. The increased resistance to breathing during sleep causes fragmented sleep. They experience symptoms such as daytime lethargy and sleepiness.
UARS causes the airway to be partially blocked by a collapse of soft tissue at the back of the mouth, and the flow of air may be minimized enough to cause arousal during sleep. There are often specific structural characteristics in patients with UARS, including a narrow palate at the back and an overjet in the bite.
After a thorough diagnostic process which includes a home sleep test and a CBCT scan, Dr. Rokadia analyses where your potential obstruction may arise from.

Treatments offered:
All types of sleep apnea have traditionally been treated with just CPAP or surgery.
While both options are valid, the compliance rate for CPAP is very low, and many patients would prefer less invasive options than surgery.
Dental treatments for obstructive sleep apnea can help reposition the tongue and jaw to improve the airway and reduce symptoms. Each patient is unique, and hence, treatment is unique as well.
Here are some of the the treatments Dr. Rokadia offers for sleep apnea:
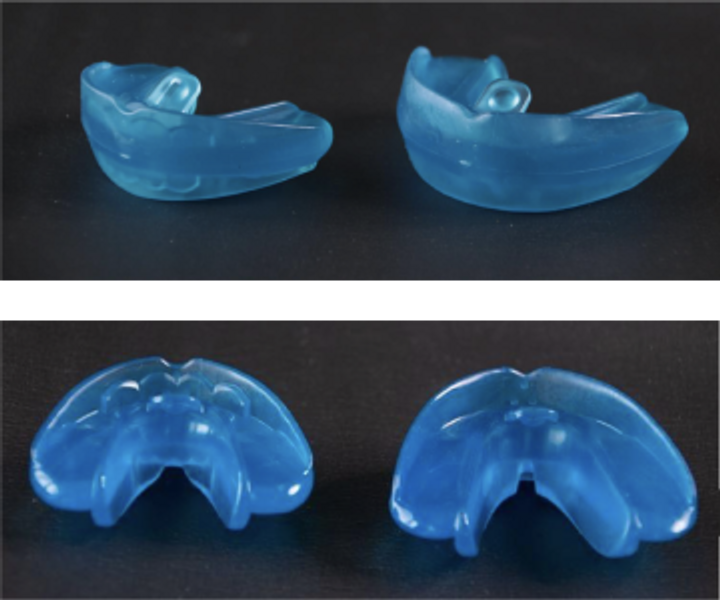
1. Oral appliances
These are custom-made mouthpieces that are worn during sleep to help reposition the jaw and tongue, and keep the airway open. Oral appliances are easy to wear and can be a good alternative to CPAP machines.


2. Myofunctional therapy
Myofunctional therapy focuses on retraining the muscles of the mouth and throat to work properly, which can help to improve breathing and reduce the risk of sleep apnea. The therapy involves exercises that are designed to strengthen the muscles of the tongue, lips, and throat, and to improve overall oral posture.
To watch a video on Myufunctional therapy click here
3. TONGUE-TIES
Updated knowledge on tongue-ties and their relation to sleep disordered breathing and sleep apnea.
4. Collaboration with ENT’s
Working in close collaboration with ENTs to perform DISE studies and explore the best options for patients.
5. SLEEP TESTS
We offer Home Sleep Studies which allow us to diagnose the presence and severity of Sleep Apnea. This is very close in accuracy to a hospital sleep study (PolySomnogram). You can use the device at home and Dr. Rokadia will discuss the results with you.





What is a tongue-tie ?
Restrictive lingual frenulum, also known as ankylglossia or tongue-tie, is a condition where the tongue is tethered to the floor of the mouth and can limit the mobility of the tongue.
The tongue plays an important role in speech, swallow, sleep, and breathing and adequate tongue mobility is essential for optimal growth and development of the upper and lower jaws.

Tongue-ties are graded based on the level of restriction of the tongue. It is also divided into anterior and posterior tongue ties depending on the part of the tongue it affects.
Tongue-ties are based on function rather than appearance and hence a simple look in the mouth cannot diagnose a tongue-tie.
Tongue-ties have a genetic component and are often missed due to lack of practitioner awareness.
This condition is not new, however the scientific research available to us has significantly increased in the last decade. Not all practitioners were taught this in their education and are frequently not updated on latest evidence-backed protocols.
Why do Tongue-Ties Matter ?
Does your older child…
- Grind teeth at night, snore, or sleep with his or her mouth open?
- Has no spacing in the baby teeth or a narrow upper arch with crowded teeth ?
- Exhibit slow or picky eating?
Choke or gag on liquids or foods? - Sleep restlessly?
- Speak softly (mumble) or struggle to be understood?
Do you ?
- Grind your teeth or have Temperomandibular joint soreness?
- Snore or suffer from reflux when asleep ?
- Wake up tired after a full nights rest ?
- Have neck and shoulder pain, mobility issues or forward head posture ?
- Have a narrow upper jaw which needed orthodontics in the past ?
Because the mobility of the tongue is restricted in the tongue-tie condition, the back of the tongue takes a posterior and inferior position which can block the airway and cause problems with sleep.
These individuals often complain of
Effective release of a lingual with restoration of tongue mobility, tongue, and posture in these individuals can have a profound impact on many areas of the person’s life.
HOW DO WE TREAT TONGUE-TIES ?
Dr. Rokadia believes in the team approach for the treatment of tongue-ties.
Myofunctional therapy is required before and after the release for the procedure to be accurate and effective Without myofunctional therapy, inadequate releases are very common. Infact, sometime the scarring from a procedure can make situation worse when myofunctional therapy is not used.
We have a multidisciplinary protocol of functional frenuloplasty that integrates myofunctional therapy (and sometimes craniosacral therapy) both before, during, and after surgery. Our technique is based on precision: releasing the appropriate extent of tissues for maximal relief; not too much, and not too little.

before

1 week healing
How do we perform frenuloplasty: with laser or scissors?
The success in our practice is based on our ability to provide a complete and effective release of tethered oral tissues. This is done with a combination of laser and scissors. Sutures are always placed at the end.
REMEMBER: It is the provider skill that matters, not the tool they use.

Dr. Rokadia is trained by The Breathe Institute on the diagnosis and treatment of tongue-ties and lip-ties.

Have a Question? Call us Now
Need Help? Drop us an Email
Visiting Hours:
Saturday to Thursday 8:00 AM – 8:00 PM
Location
Villa 733, Jumeirah Rd, Umm Suqeim 2, Dubai, U.A.E.
Have a Question? Call us Now
Need Help? Drop us an Email
Visiting Hours:
Saturday to Thursday 8:00 AM – 8:00 PM
Location
Villa 733, Jumeirah Rd, Umm Suqeim 2, Dubai, U.A.E.

